Tuesday, 21 May 2019
Libre update
While I was away in Brazil and for the last four blog posts, it's been quite an exciting time in the world of diabetes. The Libre flash glucose monitoring system, which a few short weeks ago was almost unobtainable, has now become very obtainable indeed.
There have been new (draft) guidelines that are much more inclusive than the previous ones, so that instead of almost nobody being eligible, almost everyone meets the criteria now. There has been a meeting attended by someone from the Trust who says we can go ahead and start as many people on it as we like, despite the guidelines only being in draft.
The situation is not completely relaxed though, because there is supposed to be some sort of monitoring and review of our patients to whom we give the Libre to make sure that it is having the positive effect that is claimed for it. Understandably the CCG does not want people to have a new and expensive bit of kit and then not get the benefit, which from their point of view involves a cost saving due to better blood glucose management reducing long-term health complications, and fewer prescribed blood glucose monitoring strips.
We are planning to use an online dashboard to collect information for us to review, whereby patients upload the data from their devices and we view lots of lovely graphs as well as recording auditable data. We can then report back to the CCG and support patients who are getting good results while recommending the withdrawal of the device from those who aren't using it or aren't getting any benefit or aren't using fewer strips.
And there has been a meeting with the suppliers, who gave us all a handset and sensor to wear for the next two weeks. I was delighted to be able to try some of the technology on my own non-diabetic body, although my nurse colleagues weren't very keen at all. We're all very used to looking at blood glucose results from our diabetic patients and being asked whether they are cause for concern without knowing anything about what is 'normal'. How high does blood glucose go after a high-carb meal when you haven't got diabetes? I was about to find out.
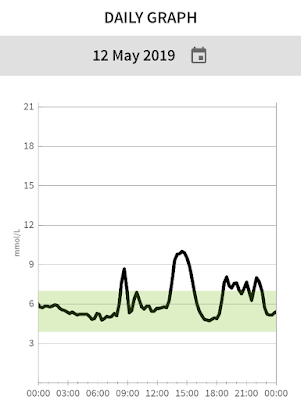
I managed to upload my data from the device (which wasn't anywhere near as straightforward as the suppliers led us to believe), and I even registered as a pretend patient with our service so that in theory I should be able to see my data both as a patient and as a Healthcare Professional. We all enthusiastically checked our glucose levels, and it has been mightily interesting. We used to say that without diabetes, fasting blood glucose levels are normally between 4 and 7 mmol/L, but we've never really known what a 'normal' post-prandial peak looks like, although pregnant women are set a threshold of 7.8 mmol/L one hour after a meal.
It turns out that our post-prandial peaks are often much higher than this - I managed to reach 12 mmol/L after a particularly nice lunch - but we do tend to come back down very quickly and stabilise within range. We also found that the sensor told us that we all drop below 4 mmol/L at some point in the night, which for someone with diabetes is classed as an unwanted night time hypo. The Libre license requires you to check blood glucose at hypo levels, but I couldn't check the 'real' state of affairs because I didn't have any blood glucose testing equipment, which someone with diabetes would have.
It was all going well and I was looking forward to seeing what happened when I played badminton, except that on Sunday night, after less than a week, the sensor came off when I removed my jumper. So that was disappointing, but it's also useful information to know that the glue isn't quite as sticky as we would hope. When I came back to work, I found that my nurse colleagues had become bored of the whole thing and had deliberately taken their sensors off after less than a week. More useful information about how patients might behave.
Then, about a week later, I was chatting to the paediatric diabetes team, and they told me that there was a stash of sensors in the department that I didn't know about. This time I put one on the other arm, and it has been behaving rather differently. It no longer shows overnight low glucose, in fact overnight is a very stable time when I sit comfortably around 5 mmol/L. So either there is a variation in the sensitivity from one sensor to another (Mr M's theory) or it matters which arm hosts the sensor because pressure on the sensor during the night is likely to confound its sampling.
So I did get to wear a sensor for badminton after all, and nothing whatever happened - no downward trend in the glucose level at all. Managing carbohydrate, insulin and blood glucose around exercise is one of the things that people who inject insulin find very difficult to manage, and the rest of us don't even notice.
I have three days to go on the second sensor, and in fact I'm now checking it less often and finding the results less interesting. The first group of actual patients with Type 1 Diabetes have now been given their sensors - unsurprisingly, everyone who had been invited turned up - and I think the second group session in June is already full. We anticipate that after this initial spike in demand everyone who wants one will have one, and we can go back to normal levels of patient apathy and non-attendance.
Labels:
diabetes,
technology
Subscribe to:
Post Comments (Atom)


Next stage (disambiguation)one person wears two sensors, one on each arm, and see which hypothesis receives confirmation (if any). Fascinating that the drop during the night followed by a rise towards morning is something that some professionals are aware and others deny. If all of you found this drop occurs, it suggests your second sensor is in error. Research - it's wonderful.
ReplyDelete